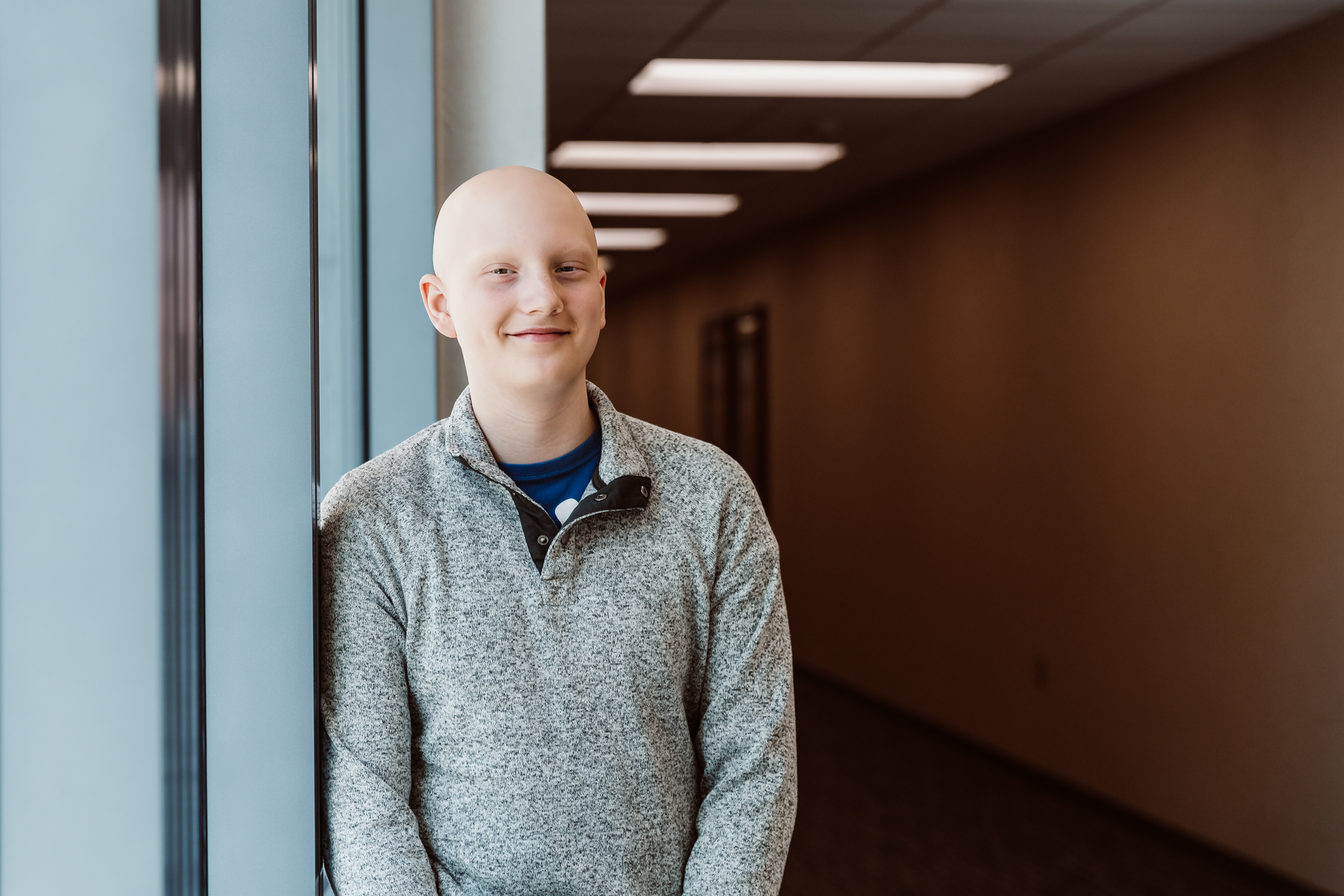
Bolton’s Bravery
With specialized, comprehensive care in hospitals tailored to the unique needs of pediatric patients, children’s hospitals help children and teens like Bolton defy the odds.

Every day, children’s hospitals help make moments possible. From providing access to the comprehensive care that children need to grow up to supporting children, teens, and their families with specialized treatment for some of the most complex illnesses. Discover more about the moments made possible by children’s hospital through patient stories from around the country.
With specialized, comprehensive care in hospitals tailored to the unique needs of pediatric patients, children’s hospitals help children and teens like Bolton defy the odds.

Children’s hospitals provide advanced care for the most complex conditions in environments specially designed for pediatric patients, allowing children like Isaac to thrive.

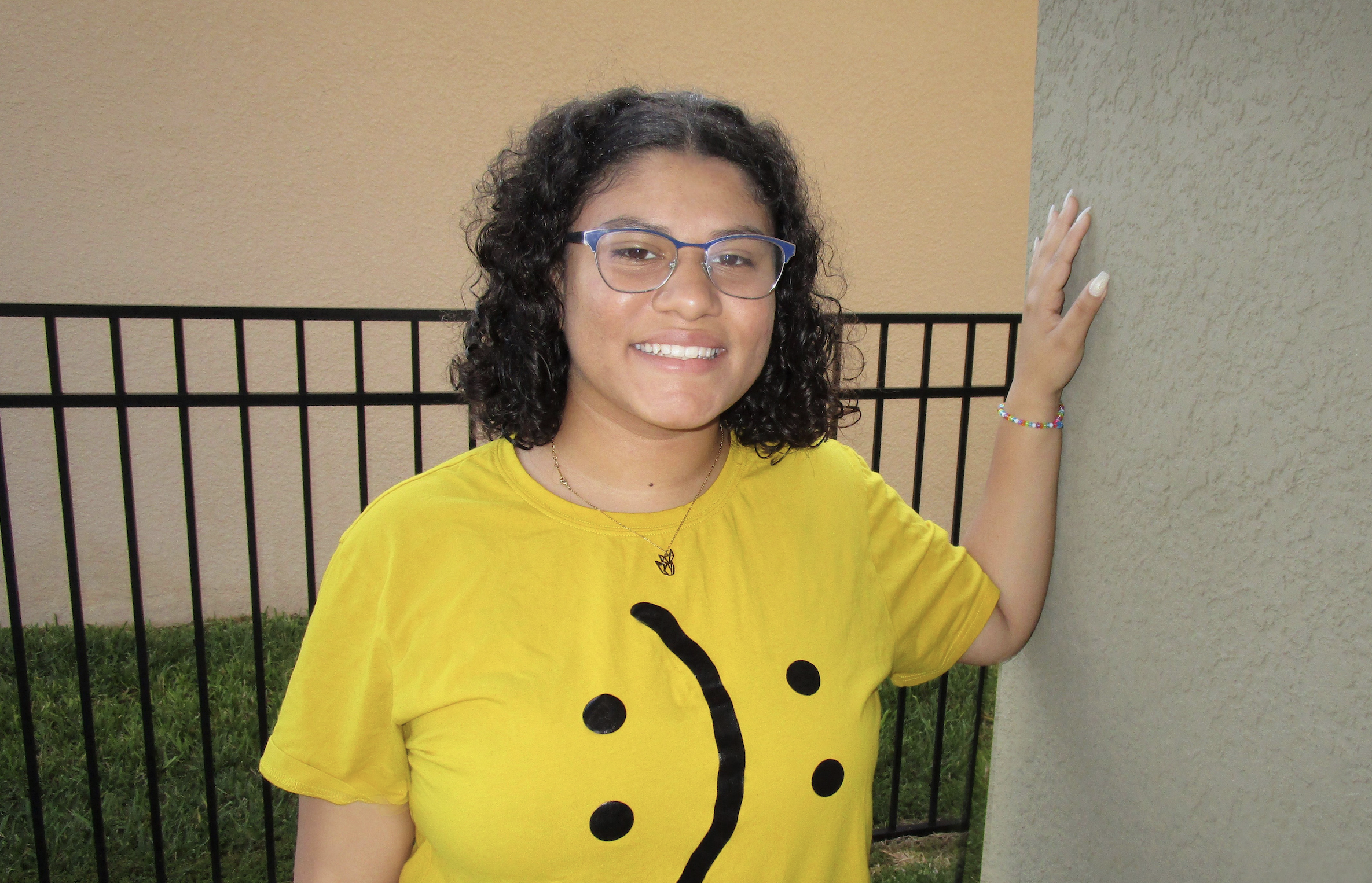
The specialized multidisciplinary teams at children’s hospitals ensure that children and teens – like Cami – can beat multiple complex conditions like cancer and heart failure.

The advanced, specialized care that children’s hospitals provide make moments – like Joseph beating pediatric brain cancer – possible.

With care delivered by specially trained pediatric clinicians, in environments designed just for children, children’s hospitals help children and teens – like Daniella – navigate complex medical conditions.

When Sriansh was just three months old, his family grew concerned as he slept most of the day, arched his back, and could not control his eye movement. His parents brought him to Cincinnati Children’s, where he was diagnosed with AADC deficiency, a rare genetic disorder that disrupts dopamine and serotonin production in the brain. Sriansh’s family was told he might never walk, talk, or lift his head. But thanks to an experimental gene therapy clinical trial, his story took a groundbreaking turn. At just 16 months old, Sriansh became the youngest child in the world to receive a one-time gene therapy treatment, delivered directly into the brain through a minimally invasive surgical technique. His care team inserted an engineered virus carrying the missing gene, allowing his brain to begin producing the essential chemicals it lacked. Today, Sriansh is walking, running, and thriving because of this innovative clinical trial. This pioneering work helped lead to the first-ever FDA-approved gene therapy administered directly to the brain, offering hope for patients with rare genetic diseases once thought untreatable.

Amanda and Rob Calvin were set to welcome their first child as Rob navigated a challenging pancreatic cancer diagnosis. Due to complications from a pre-existing bleeding disorder and preeclampsia, Amanda delivered baby Finn prematurely. He weighed just 3 pounds and 13 ounces. Following months of care in the NICU at Children’s Minnesota, Finn qualified for a new one-of-a-kind program called The Kid Experts® At Home. Families are provided with a scale and a tablet equipped with an app that allows parents to input vitals that are then shared and monitored remotely by the baby’s neonatal team. Finn got to go home a month early, giving the family valuable time together with Rob. Finn has graduated from the program. He’s walking, hitting other major developmental milestones, and making new memories every day with his mom.

Lori and Clay Smothers were overjoyed when they found out they were expecting a baby. Shortly after, the excitement turned to fear when an omphalocele – a birth defect of the abdominal wall that causes some organs to grow outside the body – was identified during a 12-week ultrasound. Le Bonheur Children’s Hospital’s Fetal Center monitored Lori closely throughout her pregnancy and helped make Easton’s delivery possible. Shortly after his birth, Easton was transferred to Le Bonheur’s NICU and was under the care of the hospital’s pediatric subspecialists until he was 19-months old and his omphalocele was surgically repaired. He is now 6 years old and loves spending time outside with his dad!

Joen was born with several complex medical conditions that needed immediate specialized care. He was born with a cleft lip, ear malformations, a heart defect, and encephalocele, a hole in the bone of his head. The El Paso Children’s Hospital was able to treat each one of Joen’s conditions because of the multidisciplinary teams that have been created, allowing a level of specialized care that did not exist in the area before. After several treatments and surgeries, Joen is thriving, meeting all of his milestones and enjoying life alongside his brothers and family in El Paso.
Lizzy was 17 and needed support to get mental health care treatment. She had to wait in an emergency room for several hours while waiting for a bed to be available, often called “boarding.” The emergency room was not designed to meet Lizzy’s mental health care needs long-term, but she eventually found the specialized care she needed at a behavioral hospital. Lizzy and her family are passionate about advocating for more mental health facilities that are reachable and in local communities.

At 3 months old, Phoenix was diagnosed with Marshall-Smith Syndrome, an ultra-rare genetic disorder that only 56 people in the world have been diagnosed with. Most children with Marshall-Smith Syndrome don’t live past age 3. Phoenix is now 9. The care that Phoenix receives at Children’s Wisconsin has been paramount to her survival. She sees gastroenterology specialists, pulmonary and otolaryngology specialists, as well as the plastic surgery and complex care team to coordinate specialty care needs. With complex care needs, Medicaid helps cover Phoenix’s regular clinic visits and medical care, but there are often challenges getting special equipment she needs covered. Despite all of the obstacles she faces, Phoenix attends school and she loves art and music.

Zachary is a celebrated concert oboist, a skill that he has preserved to perfect since a young age. That same drive to preserve has helped Zachary as he has dealt with multiple health conditions throughout his life, starting with seizures at age three, and then a systemic lupus erythematosus diagnosis at age 16 following a stroke, along with mixed connective tissue disease, CNS vasculitis and arthritis. He spent a week in the ICU and further time in the hospital and had to resume remote learning due to his autoimmune diagnosis. These were challenging setback for a teenager who was ready to get back to normal after COVID-19. Zachary has regular rheumatology appointments and bloodwork to track the progression of the diseases. Today he is in remission and has been able to resume most of his regular activities, including playing the oboe.