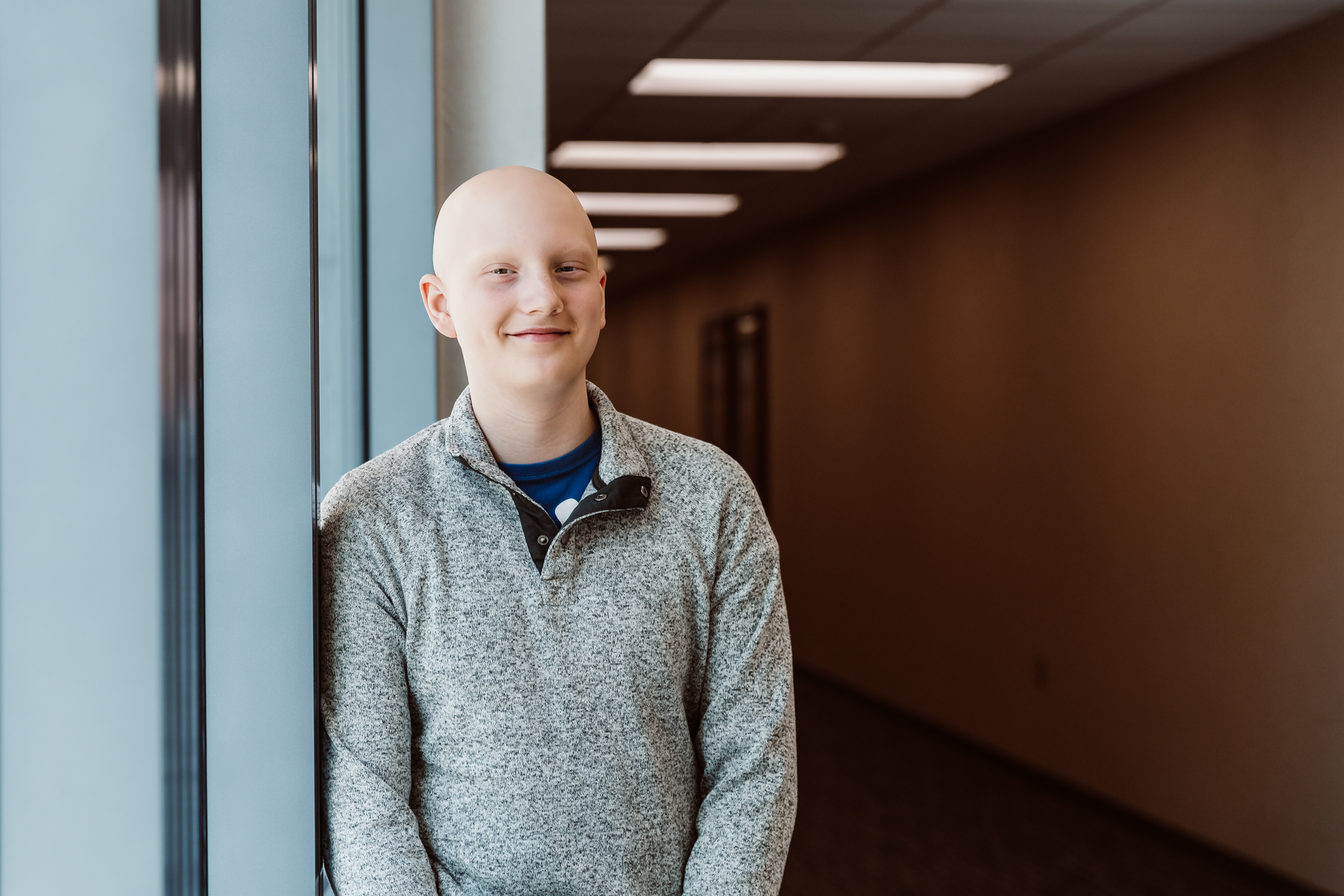
Bolton’s Bravery
With specialized, comprehensive care in hospitals tailored to the unique needs of pediatric patients, children’s hospitals help children and teens like Bolton defy the odds.

Every day, children’s hospitals help make moments possible. From providing access to the comprehensive care that children need to grow up to supporting children, teens, and their families with specialized treatment for some of the most complex illnesses. Discover more about the moments made possible by children’s hospital through patient stories from around the country.
With specialized, comprehensive care in hospitals tailored to the unique needs of pediatric patients, children’s hospitals help children and teens like Bolton defy the odds.

Children’s hospitals provide advanced care for the most complex conditions in environments specially designed for pediatric patients, allowing children like Isaac to thrive.

The specialized multidisciplinary teams at children’s hospitals ensure that children and teens – like Cami – can beat multiple complex conditions like cancer and heart failure.

The advanced, specialized care that children’s hospitals provide make moments – like Joseph beating pediatric brain cancer – possible.

With care delivered by specially trained pediatric clinicians, in environments designed just for children, children’s hospitals help children and teens – like Daniella – navigate complex medical conditions.

When Sriansh was just three months old, his family grew concerned as he slept most of the day, arched his back, and could not control his eye movement. His parents brought him to Cincinnati Children’s, where he was diagnosed with AADC deficiency, a rare genetic disorder that disrupts dopamine and serotonin production in the brain. Sriansh’s family was told he might never walk, talk, or lift his head. But thanks to an experimental gene therapy clinical trial, his story took a groundbreaking turn. At just 16 months old, Sriansh became the youngest child in the world to receive a one-time gene therapy treatment, delivered directly into the brain through a minimally invasive surgical technique. His care team inserted an engineered virus carrying the missing gene, allowing his brain to begin producing the essential chemicals it lacked. Today, Sriansh is walking, running, and thriving because of this innovative clinical trial. This pioneering work helped lead to the first-ever FDA-approved gene therapy administered directly to the brain, offering hope for patients with rare genetic diseases once thought untreatable.

After working with medically fragile infants as an emergency room tech, Bree McCarty was quickly inspired to become a foster parent for children with unique health needs. She and her husband, Tim, began fostering 4-month-old Carlos. While they didn’t have much information about Carlos’ complex medical needs, Mary Bridge Children’s neonatal follow-up clinic discovered he had hydrocephalus and was missing part of his brain. Carlos underwent multiple surgeries, including surgery to relieve the pressure on his brain and open-heart surgery. He also received a G-tube for nutrition. Carlos graduated from the neonatal follow-up clinic at 3 years old. Shortly after, the McCarty family celebrated Carlos’ long-awaited adoption and are thrilled to continue their life together. Continuing his care journey, Carlos works with therapists at the Mary Bridge Children’s Therapy – Puyallup and is now a bubbly 5-year-old who is thriving. Carlos is learning to walk and loves kindergarten, his siblings, and making people laugh. His parents say his adorable dimples help him get away with goofing around!

Monroe Carell Jr. Children’s Hospital at Vanderbilt recently introduced Angel 7, a first-of-its-kind ambulance in Tennessee. Angel 7 is the first ambulance in its group to offer extracorporeal membrane oxygenation (ECMO), a type of life support that provides oxygen to the heart and lungs in severe situations. While most patients can only receive ECMO once they arrive at a hospital, Angel 7 allows the team to provide this critical care for pediatric patients, like 5-year-old Gracie Conlon, while transporting them to Monroe Carell. Gracie suffers from an atrioventricular septal defect (AVSD). Earlier this year, she was exhibiting severe symptoms and needed ECMO support, but she was 200 miles away from the nearest ECMO center. Fortunately, Angel 7 was able to transport her while simultaneously providing the critical care that saved her life. Angel 7 has changed the course of critical care in Tennessee and will help more pediatric patients sooner and throughout the transport process.
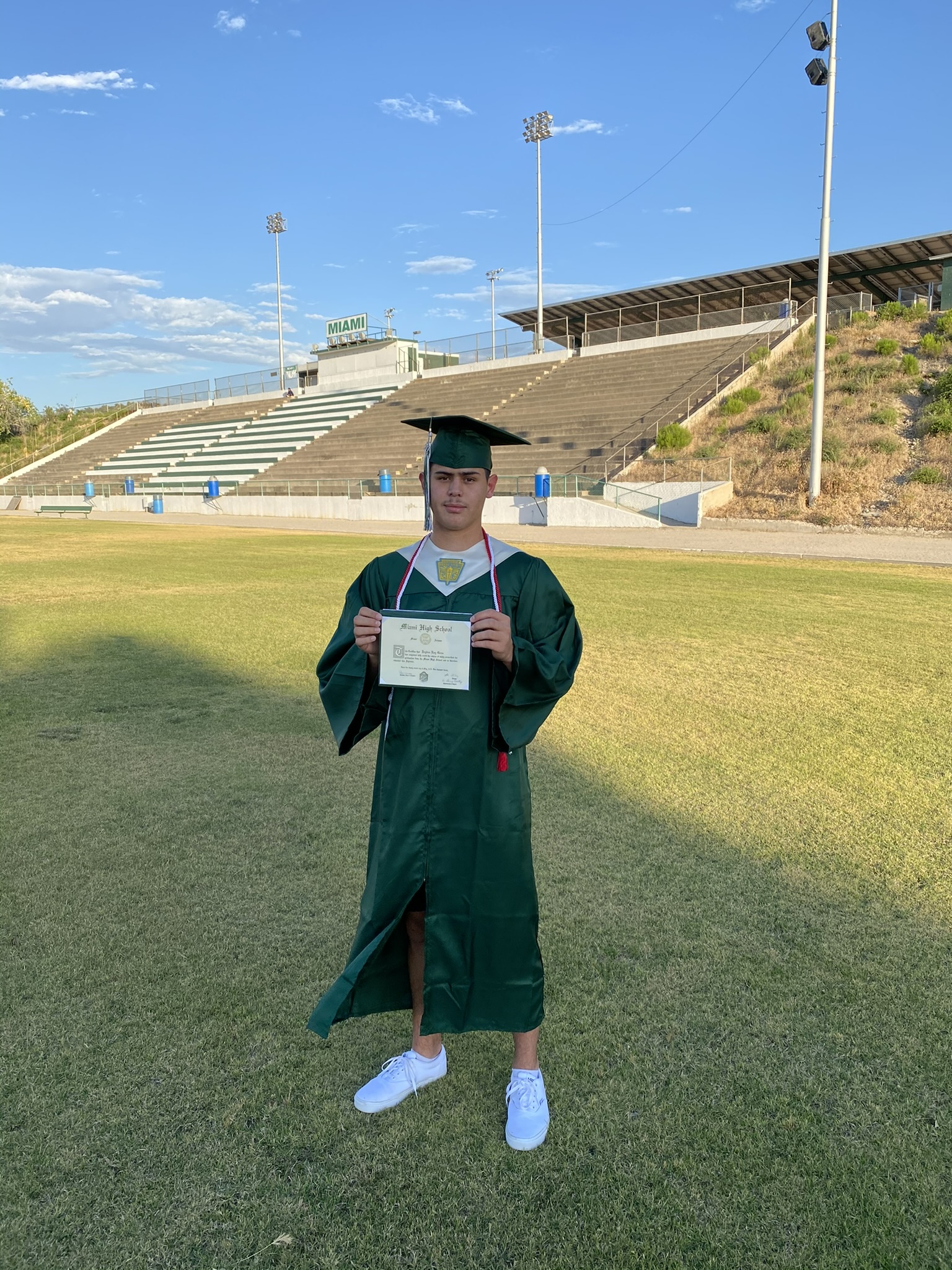
Like many other college students, Jayden Goss was attending an Arizona State University basketball game. But as he was waiting for the game to start, he suddenly stopped being able to form words. Jayden soon discovered he had experienced a stroke. He struggled to find hospitals that could help him, but eventually Jayden wound up at Phoenix Children’s where they took a closer look at his heart. They diagnosed Jayden with three rare congenital heart defects that he had lived with since his childhood without knowing. Jayden underwent open heart surgery and later got a tattoo of his surgery date to commemorate this life-changing time. Phoenix Children’s is the only Adult Congenital Heart Disease (ACHD) treatment program in Arizona and the Southwest. While Jayden had to miss a whole year of college, he is ecstatic to return to ASU in the Spring of 2024.

In early 2023, St. Louis Children’s Hospital launched the country’s first-ever mobile pediatric diabetes unit. The Healthy Kids Express Diabetes Mobile Unit now travels to schools, where Washington University Physicians provide care to diabetic children while educating them on how to manage their condition. The mobile unit’s team trains school nurses to administer insulin shots and glucose monitoring machines to support children in the classroom. St. Louis’s diabetes mobile unit is also helping to overcome socioeconomic barriers by delivering care to children in low-income areas who may have limited access to healthcare and healthy foods. As diabetes continues to be one of the most common chronic diseases among children, this traveling unit is incredibly essential. The Healthy Kids Express Diabetes Mobile Unit will continue to bring necessary and accessible diabetic care to children across northern St. Louis County. This unit was made possible thanks to generous donations to the St. Louis Children’s Hospital Foundation.

Two days after Kitson was born, doctors discovered an open atrioventricular canal in her heart—a familiar yet frightening condition that commonly impacts infants with Down Syndrome. Filled with confusion and fear, Kitson’s family found themselves at Cook Children’s Health Care System in Fort Worth five months later, where the Cardiac Intensive Care team met them with open arms. As they operated on her for several hours, the team went the extra mile to comfort Kitson’s family as they paced the hospital awaiting news. But after a successful surgery, she quickly developed pulmonary hypertension. The care team returned to the drawing board, carefully tailoring a treatment plan that helped her lungs become strong again. Throughout Kitson’s journey, the staff never hesitated to make her family feel loved and encouraged, providing a circle of support when they needed it most. Kitson is now back home in New Mexico, a happy and spunky baby. The team at Cook Children’s continues to offer guidance from afar and will forever hold a special place in the Bell family’s hearts.

As Sara and Dan awaited the delivery of their first child, Hayden, an update from the Doctor brought a sudden turn of events. Their anticipated 7-pound baby would enter the world at 9 pounds. When babies like Hayden are bigger, they pose more challenges during labor and are at higher risk of developing brachial plexus birth palsy – a condition when the nerves from the neck down to the arm and hands can become injured during birth. At Hayden’s two-month check-in, he was diagnosed with brachial plexus birth palsy and began daily physical therapy at the UPMC Children’s Hospital of Pittsburgh’s Brachial Plexus Clinic. As he made notable progress at physical therapy, he hadn’t entirely regained full range of motion, and doctors decided surgery would be the next best step. Hayden championed his 6-hour reconstructive surgery and attended routine check-ups over the next year. After an incredible recovery, 3-year-old Hayden is no longer limited by functional issues and enjoys climbing, swinging, and playing outside!