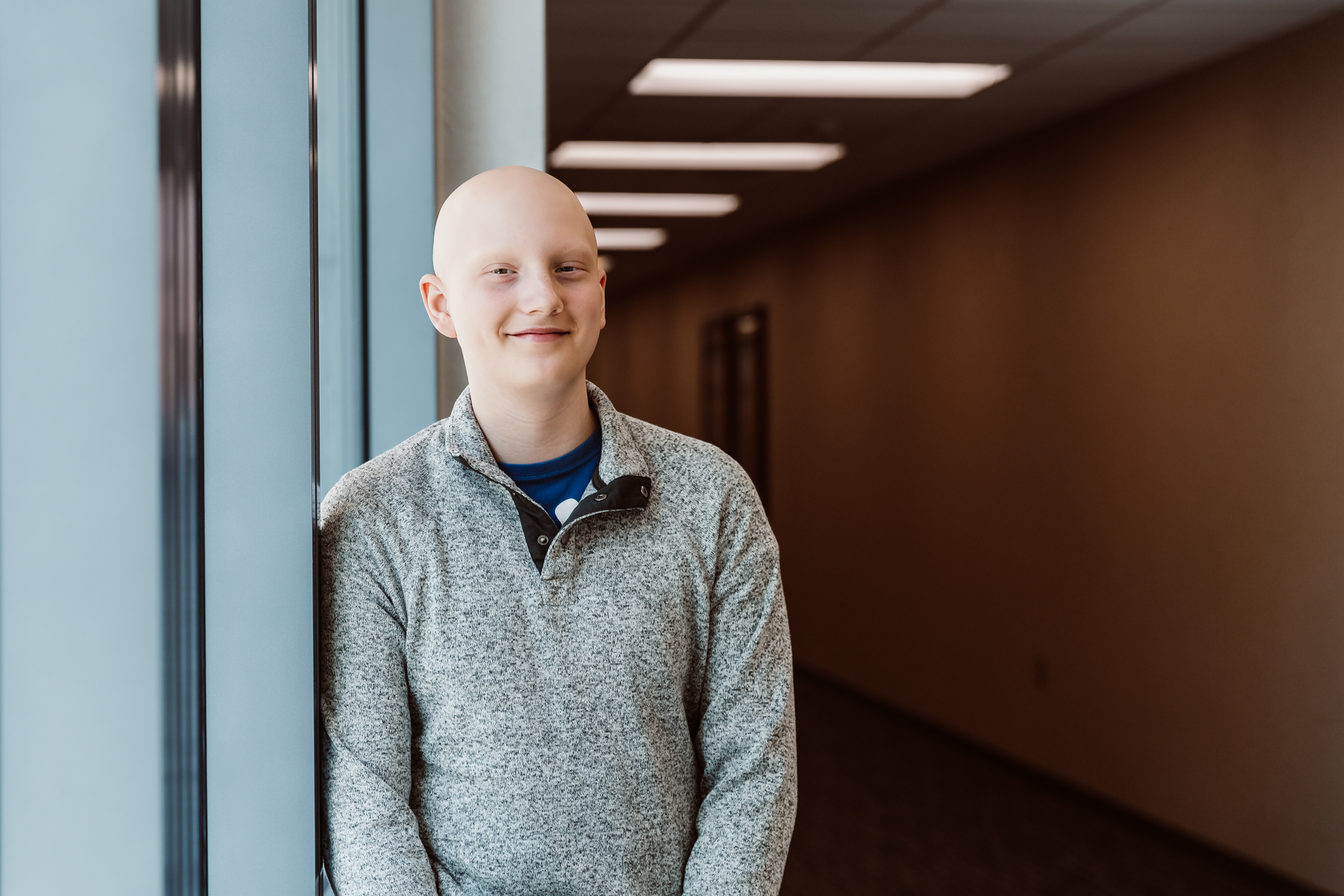
Bolton’s Bravery
With specialized, comprehensive care in hospitals tailored to the unique needs of pediatric patients, children’s hospitals help children and teens like Bolton defy the odds.

Every day, children’s hospitals help make moments possible. From providing access to the comprehensive care that children need to grow up to supporting children, teens, and their families with specialized treatment for some of the most complex illnesses. Discover more about the moments made possible by children’s hospital through patient stories from around the country.
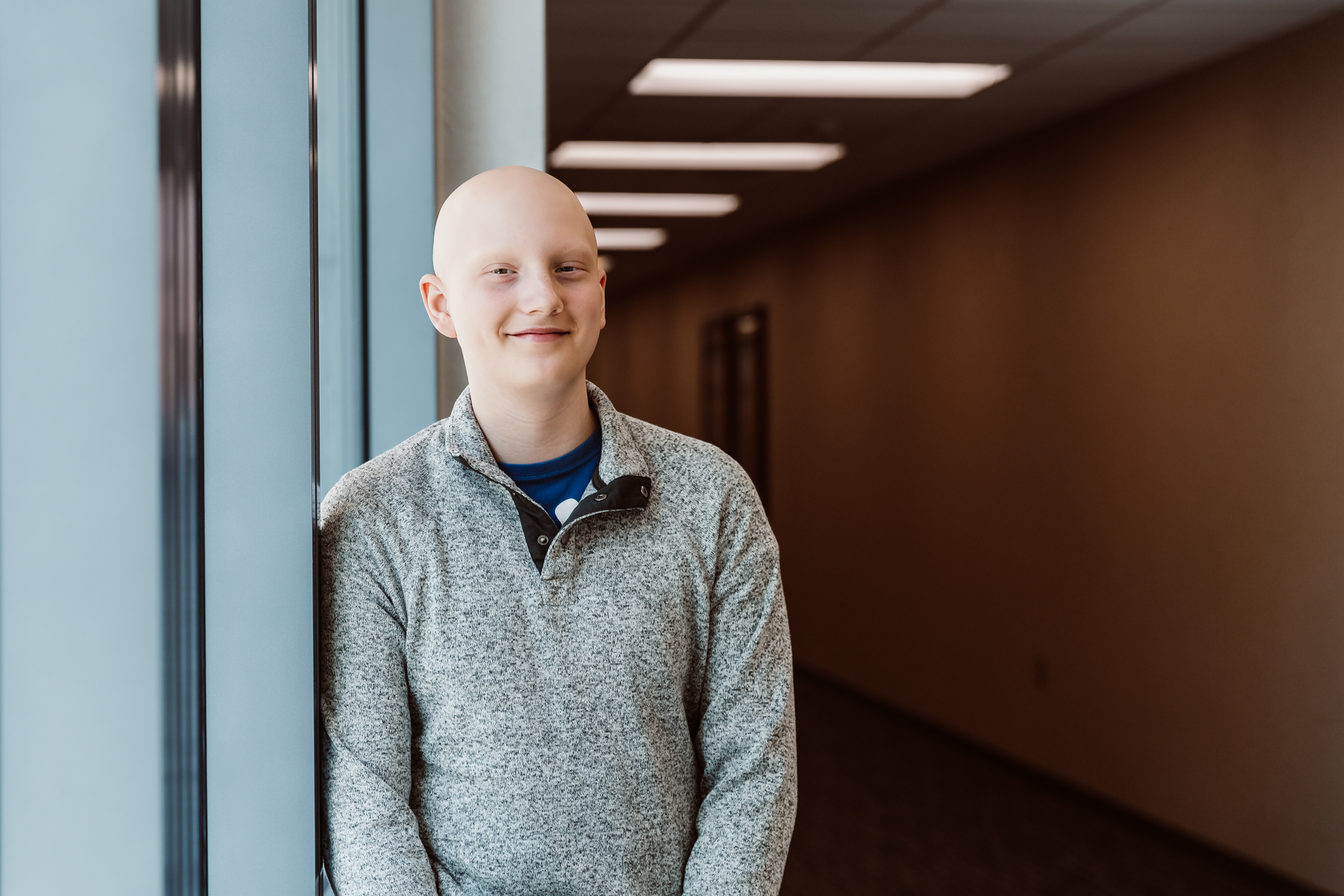
With specialized, comprehensive care in hospitals tailored to the unique needs of pediatric patients, children’s hospitals help children and teens like Bolton defy the odds.

Children’s hospitals provide advanced care for the most complex conditions in environments specially designed for pediatric patients, allowing children like Isaac to thrive.

The specialized multidisciplinary teams at children’s hospitals ensure that children and teens – like Cami – can beat multiple complex conditions like cancer and heart failure.

The advanced, specialized care that children’s hospitals provide make moments – like Joseph beating pediatric brain cancer – possible.

With care delivered by specially trained pediatric clinicians, in environments designed just for children, children’s hospitals help children and teens – like Daniella – navigate complex medical conditions.

When Sriansh was just three months old, his family grew concerned as he slept most of the day, arched his back, and could not control his eye movement. His parents brought him to Cincinnati Children’s, where he was diagnosed with AADC deficiency, a rare genetic disorder that disrupts dopamine and serotonin production in the brain. Sriansh’s family was told he might never walk, talk, or lift his head. But thanks to an experimental gene therapy clinical trial, his story took a groundbreaking turn. At just 16 months old, Sriansh became the youngest child in the world to receive a one-time gene therapy treatment, delivered directly into the brain through a minimally invasive surgical technique. His care team inserted an engineered virus carrying the missing gene, allowing his brain to begin producing the essential chemicals it lacked. Today, Sriansh is walking, running, and thriving because of this innovative clinical trial. This pioneering work helped lead to the first-ever FDA-approved gene therapy administered directly to the brain, offering hope for patients with rare genetic diseases once thought untreatable.

While Hudsyn was born healthy, once he was a few months old, he became increasingly uncoordinated, had weak muscle tone, and suffered migraines. His mom took him to Mary Bridge Children’s, where an MRI exposed syringomyelia, a fluid-filled cyst that grows in the spinal cord and can impact nerves. After the diagnosis, he underwent his first brain surgery, which didn’t alleviate his symptoms very much. About a year later, Hudsyn returned for his second brain surgery. Following this surgery, he relearned how to walk in physical therapy, but his migraines returned. A few months later, at only four years old, he underwent this third and most successful brain surgery. His surgeon guided him through each step of the way, forming an unbreakable bond with Hudsyn. After the third procedure, Hudsyn worked hard at physical therapy to relearn how to walk again. With determination and persistence, he finished physical therapy and was cleared to play sports! Now, he loves throwing balls and running but enjoys playing T-ball most of all. When he’s not playing ball on the field, Hudsyn loves dressing up as a doctor at home!

11-year-old Morgan began to have constant stomach pain, and doctors struggled to determine the cause. After months of pain, it became so unbearable that her parents took her to the ER. A worrisome CT scan led to an MRI and various lab work that ultimately revealed a potentially cancerous tumor on her pancreas. While this tumor is not uncommon in young women, they aren’t typically found in children as young as Morgan. Her care team at her community hospital in Virginia determined she would need the Whipple procedure, and Children’s Hospital of Richmond at VCU (CHoR and VCU Health) stepped in to help. Before her 7-hour surgery, doctors and child life specialists made sure Morgan felt comfortable and prepared. They even encouraged her to partake in her favorite activity, hunting, the day before her surgery. The surgery went well, and Morgan went home after just three days, and by the next week, she was hunting again! Her tumor was completely removed, and she won’t need any future treatment.

Rahul was preparing to enter his senior year of high school when a serious motorcycle accident dramatically changed his life. Rahul sustained a severe traumatic brain injury (TBI) and was quickly brought to Blythedale Children’s Hospital’s Traumatic Brain Injury Unit for comprehensive rehabilitation. When he first arrived, he was in a disorder of consciousness, preventing him from fully responding to his environment. Over time, he rebuilt his strength and cognition with intensive physical, occupational, speech, and feeding therapies. After Rahul regained his ability to talk, he began strength and core exercises that helped him walk and eventually jog again. Once he was medically stable and independently walking, he transitioned to Blythedale’s Day Hospital program, allowing him to receive care from the comfort of his home. Rahul also attended Blythedale’s onsite public school, so he could continue his education while working with therapists between classes. With the specialized care to improve his cognitive and physical abilities, Rahul made tremendous progress, and transitioned back to his regular high school where he graduated last year.

Physicians at Stanford Medicine Children’s Health developed an innovative way to provide pediatric kidney transplants without immune-suppressing drugs. This two-transplant combination is called a dual immune/solid organ transplant (DISOT) and has been used to treat patients with rare immune diseases. This new transplant method ensures that recipients do not experience immune rejection of their transplanted organ, helping facilitate successful transplants for 8-year-old Kruz and his 7-year-old sister Paizlee. Both children were born with rare immune diseases and are among the first ever to receive DISOT. Kruz received transplants from their mother, Jessica, and Paizlee received transplants from their father, Kyle. Since the transplants, both children no longer have the immune disorder and are doing things they never thought to be possible. The siblings recently finished first grade, and they are enjoying swimming lessons and going camping with their parents!

When pregnant mom, Shakiara, learned that her lupus placed her unborn child at a higher risk of congenital complete heart block, she began to receive weekly fetal checks with her care team. Her baby, Cameron, presented well until 21 weeks, when the exam indicated signs of heart block and within hours, Shakiara was seen in the Fetal Heart Program at Children’s Hospital of Philadelphia (CHOP). In most cases, children born with heart block will eventually require a pacemaker. In addition to heart block, Cameron was also born with pulmonary hypertension and abnormally rapid breathing that can make it unsafe for infants to feed orally. When Cameron’s breathing and feeding issues failed to progress, his care team agreed that a pacemaker was the right approach. Because the average pacemaker is too large for small infants, Cameron was set to receive the Medtronic Micra, the smallest available pacemaker in the world. Surgeons were able to insert this tiny pacemaker through a tiny incision, enabling Cameron to recover faster. Shakiara says from the first sign of heart block to Cameron’s successful surgery, the entire team at CHOP was there to support her and answer all her questions. Now, Cameron is home and on the road to recovery.

Ester and her husband Samuel were eagerly waiting to discover their baby’s gender when the ultrasound revealed that their baby boy had spina bifida, a condition that prevents the spine from developing correctly. The couple was connected with Timothy M. Crombleholme, MD, Fetal Surgeon at Connecticut Children’s who could perform an in-utero surgery to help correct the condition and give their son a better chance at a healthier life. Ester decided she wanted to proceed, so she, Samuel, and their daughter Rebecca traveled from their home in Oregon to Connecticut for the surgery. The surgery went well, but a few weeks later, Ester returned to the hospital with severe bleeding; it turned out she was going into labor early and had to have a C-section. Immediately after birth, their newborn, Thaddeus, went straight to the NICU. At first, Thaddeus had no movement in his legs, but after a few weeks in the NICU, he could move around and showed signs of significant improvement. Today, the family is back in Oregon and is grateful for the care they received.